Understanding Mobile Cardiac Telemetry (MCT): A Game-Changer in Continuous Heart Monitoring
In the evolving landscape of digital health, Mobile Cardiac Telemetry (MCT) has emerged as a breakthrough technology for real-time cardiac monitoring. Offering an unmatched combination of mobility, continuity, and diagnostic accuracy, MCT systems are transforming how clinicians detect, diagnose, and manage cardiac arrhythmias. For patients at risk of intermittent or silent heart rhythm disorders, MCT offers peace of mind and early intervention in a way traditional monitoring tools cannot.
4/5/20252 min read
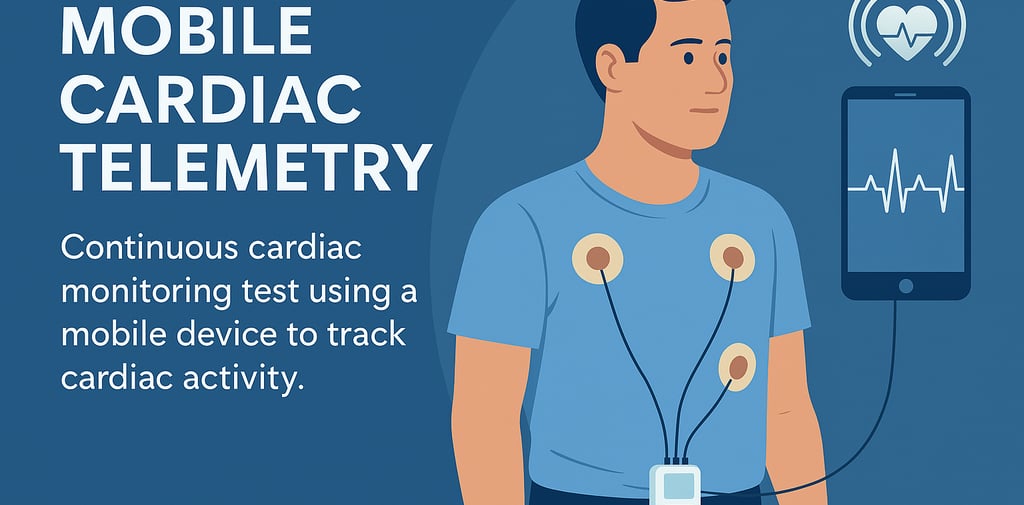
What Is Mobile Cardiac Telemetry (MCT)?
Mobile Cardiac Telemetry is an advanced form of ambulatory ECG monitoring that continuously records a patient’s cardiac rhythm and automatically transmits abnormal events to a remote monitoring center via mobile networks. Unlike Holter monitors, which record ECGs for 24–48 hours and require in-clinic data retrieval, MCT offers real-time analysis and transmission, enabling prompt clinical response.
MCT devices typically consist of:
A wearable sensor or patch that captures ECG data continuously.
A transmission device (often a smartphone-sized monitor or embedded mobile modem) that sends data to a secure cloud.
A remote monitoring center where trained cardiac technicians review the data 24/7.
How Does MCT Work?
Continuous ECG Monitoring: The device records every heartbeat for days or weeks.
Event Detection: When arrhythmias or abnormalities (e.g., atrial fibrillation, bradycardia, pauses) occur, they are automatically flagged by built-in algorithms.
Immediate Data Transmission: Detected events are sent via a mobile network to a cardiac monitoring center.
Expert Review and Clinical Notification: A trained technician confirms the event and notifies the prescribing physician, often within minutes.
Key Benefits of Mobile Cardiac Telemetry
Real-Time Monitoring and Alerts: Allows early intervention and improves patient outcomes.
Extended Monitoring Period: Typically used for 14–30 days, increasing diagnostic yield.
High Sensitivity and Specificity: Superior to Holter monitors and event recorders in detecting transient or asymptomatic arrhythmias.
Patient Comfort: Compact, wireless, and less intrusive than traditional monitors.
Compliance Monitoring: Most MCT systems track device usage and can alert clinicians to non-compliance.
Clinical Use Cases
Unexplained Syncope or Dizziness
Post-Ablation Monitoring for Atrial Fibrillation
Evaluation of Palpitations
Cryptogenic Stroke Investigation
Assessment of Ventricular Ectopy or Bradyarrhythmias
According to a 2020 study in Circulation: Arrhythmia and Electrophysiology, MCT detected clinically relevant arrhythmias in over 60% of cases where Holter monitoring had failed to capture intermittent symptoms.
MCT vs. Holter and Event Monitors
Feature Holter Monitor Event Monitor MCT Duration of Monitoring 24–48 hours Up to 30 days 14–30 days Data Transmission Offline Patient-triggered Real-time automatic Symptom Correlation Manual diary Manual + auto capture Continuous + automatic Alert System None Delayed Immediate
Limitations and Considerations
Cost and Reimbursement: MCT systems may be more expensive than traditional options, though many are covered under insurance or Medicare when clinically justified.
Network Dependence: Performance relies on cellular connectivity.
Patient Education: Proper application and wear are critical for accurate data collection.
The Future of MCT in Digital Cardiology
As AI and machine learning continue to evolve, the future of MCT includes:
Predictive arrhythmia modeling
Integration with electronic health records (EHRs)
Remote therapeutic adjustments
Greater use in preventive cardiology and telemedicine
Conclusion
Mobile Cardiac Telemetry is reshaping the paradigm of ambulatory cardiac care. Its real-time capabilities, extended monitoring, and diagnostic precision make it a powerful tool for clinicians managing patients with elusive or episodic arrhythmias. As mobile health continues to grow, MCT stands out as a life-saving advancement—merging continuous care with clinical confidence.
References:
Zimetbaum, P., & Goldman, A. (2010). Ambulatory Arrhythmia Monitoring: Choosing the Right Device. Circulation, 122(16), 1629–1636.
Turakhia, M. P., et al. (2020). Diagnostic Utility of Mobile Cardiac Telemetry in Real-World Clinical Practice. Circulation: Arrhythmia and Electrophysiology, 13(5), e008101.
Centers for Medicare & Medicaid Services (CMS). (2023). Coverage Determinations for Mobile Cardiac Telemetry.
