Personalized Cardiac Care: Setting Individual Thresholds in BodyKom
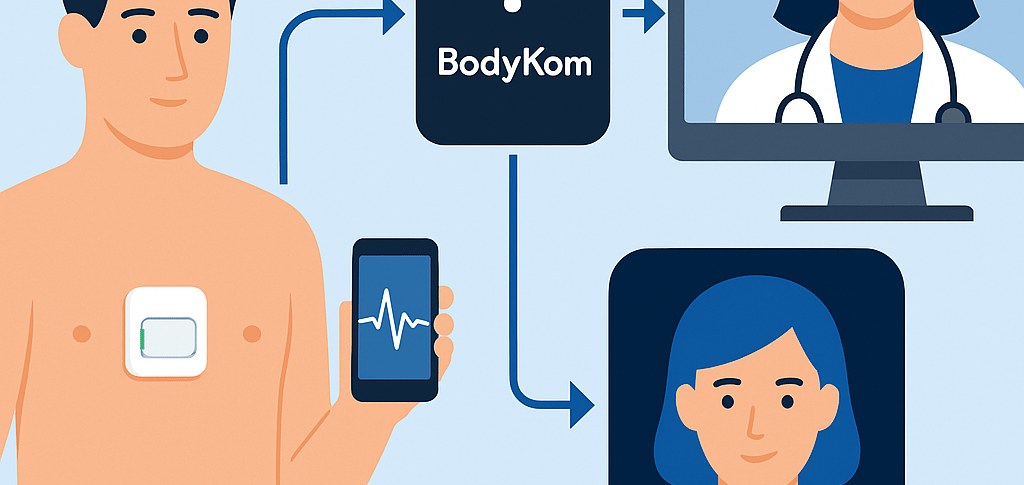
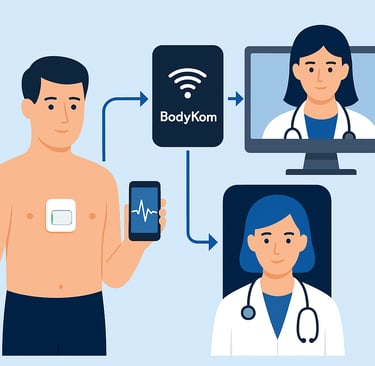
In today’s era of precision medicine, one-size-fits-all approaches are no longer sufficient—especially when it comes to managing cardiac health. BodyKom, a mobile ECG monitoring system, stands at the forefront of personalized care by allowing clinicians to set individualized thresholds for each patient’s unique cardiac profile. This customization enhances diagnostic accuracy, reduces false alarms, and supports more proactive and patient-specific clinical interventions.
4/5/20252 min read
Why Individualized Thresholds Matter
Heart rhythms and vital signs vary significantly between individuals. A heart rate of 50 bpm may be alarming in a sedentary adult but perfectly normal for a well-trained athlete. Likewise, patients with atrial fibrillation, post-myocardial infarction syndromes, or heart failure may each require different monitoring strategies.
By enabling clinicians to customize alert parameters—such as heart rate limits, arrhythmia patterns, ST-segment deviations, and QT intervals—BodyKom ensures that the system only flags events that are clinically relevant to the patient. This personalization helps prioritize alerts that truly require medical attention.
How Thresholds Are Set in Practice
Upon initiating monitoring with BodyKom, clinicians input the patient’s:
Baseline ECG characteristics
Medical history (e.g., ischemic heart disease, valvular disease)
Medication profile (e.g., beta blockers, antiarrhythmics)
Physical activity levels and known tolerance ranges
The backend system allows flexible configuration of thresholds, such as:
Heart rate upper/lower limits (e.g., >120 bpm, <45 bpm)
Number and duration of ventricular ectopic beats
Detection of atrial fibrillation or flutter episodes
ST elevation or depression thresholds
Pauses, blocks, or signal irregularities
These parameters are monitored in real time. If a reading breaches the set limits, the system triggers an automated alert to the assigned clinician or care team.
Clinical Examples
Case 1: Post-PCI Surveillance
A patient recovering from a stent placement is monitored with narrow ST-segment elevation thresholds to catch early signs of re-occlusion. BodyKom alerts the clinician to subtle ST changes, prompting timely re-evaluation.
Case 2: Elderly Patient on Rate-Limiting Medication
An 83-year-old woman with heart failure on beta blockers is set with lower bradycardia thresholds (e.g., <45 bpm). The personalized settings prevent unnecessary alarms while still catching clinically significant pauses.
Case 3: Athlete With Sinus Bradycardia
A 40-year-old endurance runner has a resting heart rate of 42 bpm. BodyKom is configured not to flag this as abnormal, avoiding redundant notifications and anxiety.
Benefits of Personalized Thresholds
Reduced alert fatigue for clinicians
Higher signal-to-noise ratio in data interpretation
Faster response to clinically meaningful events
Better patient engagement through tailored care
Future Outlook: AI and Adaptive Thresholds
Future iterations of BodyKom could leverage artificial intelligence to dynamically adjust thresholds based on evolving patient data. Machine learning models may soon be able to suggest personalized limits based on aggregated historical trends and population health data, making cardiac monitoring even more intelligent and individualized.
Conclusion
Personalized threshold setting is one of BodyKom’s most powerful features—empowering clinicians to deliver cardiac care that’s as unique as the patients themselves. By aligning technology with individualized medicine, BodyKom helps ensure that real-time monitoring is accurate, relevant, and truly life-enhancing.
