Obsolescence in Medical Equipment and Devices: Challenges, Strategies, and Best Practices
Obsolescence is a growing challenge in the medical technology industry, with significant consequences for healthcare institutions, researchers, and policymakers. The rapid pace of innovation, evolving regulatory requirements, and the short lifecycle of medical equipment create financial and operational burdens on healthcare providers. Moreover, obsolescence affects patient care, clinical outcomes, and long-term research initiatives. In this article, we explore the causes and impact of medical equipment obsolescence, industry concerns, and strategies to mitigate risks while optimizing investments.
3/31/20254 min read
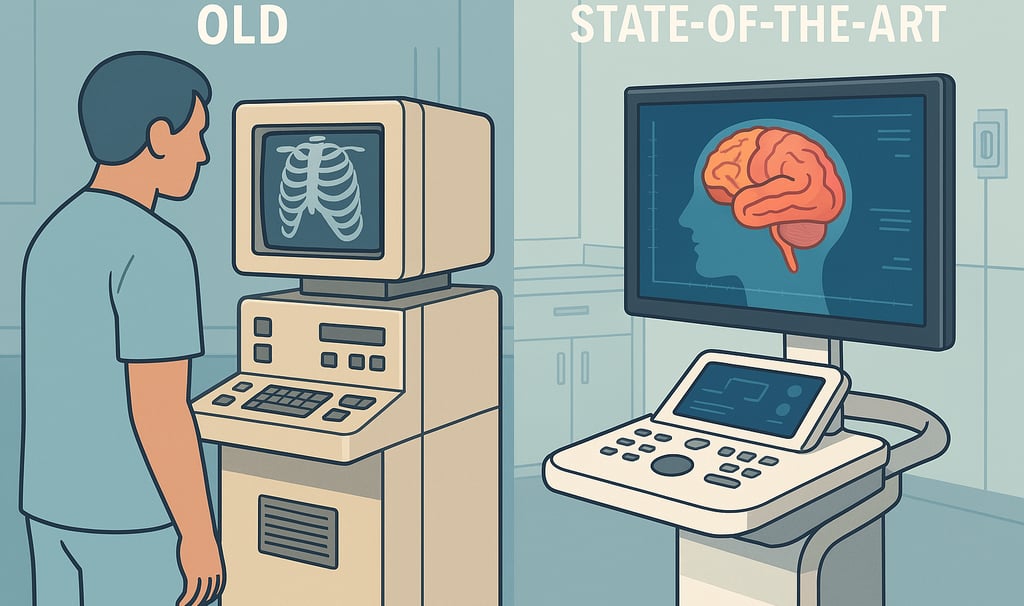
Understanding Obsolescence in Medical Equipment
Medical equipment obsolescence can be categorized into three primary types:
Technological Obsolescence: When newer, more efficient technologies replace existing devices, rendering them outdated.
Regulatory Obsolescence: When compliance requirements change, making previously approved equipment non-compliant.
Functional Obsolescence: When devices become difficult or costly to maintain due to a lack of spare parts or software updates.
Several high-profile cases highlight the risks associated with obsolescence. For example, a paralyzed man relying on an exoskeleton faced significant challenges when his device became too old for continued support and service (Futurism, 2024). Similar cases have been reported in diagnostic imaging, where MRI and CT scanners become obsolete due to software incompatibility rather than mechanical failure (WHO, 2023).
Industry Concerns and Economic Impact
Healthcare institutions invest billions in medical equipment, yet rapid obsolescence leads to increased capital expenditures. According to a 2021 report by the American Hospital Association (AHA), hospitals spend an estimated $93 billion annually on medical equipment, with 30% of devices becoming obsolete within 5–10 years (AHA, 2021). The implications include:
Increased Costs: Replacing obsolete equipment requires significant financial resources, often at the expense of other critical healthcare needs.
Downtime and Service Disruptions: Older devices may require extensive maintenance, leading to prolonged downtime and patient care delays.
Environmental Concerns: Electronic waste from obsolete medical equipment poses disposal challenges, with sustainability efforts lagging behind (UNEP, 2022).
Impact on Research and Innovation
Medical research relies heavily on cutting-edge diagnostic and treatment tools. When research institutions use outdated equipment, it limits the scope and accuracy of findings. Additionally, obsolete technology discourages innovation due to incompatibility with newer methodologies.
For example, in genomic sequencing, older sequencers produce lower-resolution data, restricting advancements in personalized medicine (Collins et al., 2022). Similarly, AI-driven diagnostics require modern imaging systems, yet many hospitals still operate decade-old MRI machines incapable of integrating deep-learning algorithms (Topol, 2021).
Turnaround and Service Life of Major Medical Equipment
The lifespan of medical equipment varies significantly by category:
MRI Machines: Typically 10–15 years, but software support may cease earlier (Siemens Healthineers, 2023).
CT Scanners: 7–10 years, often limited by regulatory updates (Philips, 2022).
Infusion Pumps: 5–7 years, with cybersecurity concerns accelerating obsolescence (FDA, 2021).
Ventilators: 8–10 years, but COVID-19 highlighted the need for rapid software updates (WHO, 2023).
Strategies to Mitigate Medical Equipment Obsolescence
1. Lifecycle Management and Predictive Maintenance
Hospitals and clinics should implement lifecycle management plans to anticipate and prepare for equipment replacements. Predictive maintenance using IoT sensors can extend service life by identifying failures before they occur (Lee et al., 2022).
2. Modular and Upgradeable Design
Manufacturers should prioritize modular designs that allow hardware and software upgrades instead of full replacements. Philips and GE Healthcare have introduced upgradeable MRI platforms, reducing the financial burden on hospitals (GE Healthcare, 2023).
3. Regulatory Harmonization and Extended Certification
Regulatory agencies should consider extended certification for well-maintained devices to prolong their usability. The FDA’s Digital Health Software Precertification Program aims to facilitate software updates without extensive reapproval (FDA, 2023).
4. Refurbishment and Secondary Markets
Purchasing refurbished equipment can reduce costs while maintaining quality standards. WHO’s Priority Medical Devices Initiative supports the use of certified refurbished machines in low-resource settings (WHO, 2023).
5. Cloud-Based Software and AI Integration
Implementing cloud-based solutions allows software updates without hardware changes. AI-based diagnostics, such as IBM Watson Health, demonstrate how software-driven solutions can extend the life of imaging and diagnostic tools (Watson Health, 2022).
Case Studies in Best Practice
Case Study 1: Cleveland Clinic’s Predictive Maintenance Model
Cleveland Clinic adopted predictive analytics for medical equipment maintenance, reducing unplanned downtime by 35% and cutting maintenance costs by $10 million annually (Cleveland Clinic, 2023).
Case Study 2: NHS Refurbishment Program
The UK’s National Health Service (NHS) invested in refurbishing MRI and CT scanners rather than replacing them, saving an estimated £300 million over five years while maintaining high-quality imaging (NHS, 2022).
Case Study 3: India’s Affordable Medical Equipment Initiative
To address budget constraints, India’s healthcare sector adopted locally manufactured, cost-effective medical devices with extended support services. This strategy increased access to diagnostic tools in rural areas by 40% (India Ministry of Health, 2023).
Conclusion
Obsolescence in medical equipment remains a major challenge, impacting financial sustainability, patient care, and research innovation. While rapid technological advancements drive progress, they also create significant risks for healthcare providers. Implementing proactive strategies such as predictive maintenance, modular upgrades, regulatory harmonization, and refurbished equipment adoption can mitigate the negative effects of obsolescence. By prioritizing long-term planning and sustainable investments, decision-makers can optimize resource allocation while ensuring access to cutting-edge medical technology.
References
American Hospital Association (AHA). (2021). Hospital Equipment Expenditure Report.
Cleveland Clinic. (2023). Predictive Maintenance in Healthcare: A Success Story.
Collins, F. S., et al. (2022). Genomics and the Future of Personalized Medicine. Nature Reviews Genetics.
FDA. (2021). Medical Device Cybersecurity Report.
FDA. (2023). Digital Health Software Precertification Program.
Futurism. (2024). Paralyzed Man’s Exoskeleton Becomes Too Old for Support.
GE Healthcare. (2023). Sustainable MRI: Modular Designs and Upgrades.
India Ministry of Health. (2023). Affordable Medical Equipment Initiative.
Lee, J. et al. (2022). Predictive Maintenance in Medical Equipment: IoT Applications. IEEE Transactions on Biomedical Engineering.
NHS. (2022). Cost Savings through Refurbishment of Medical Equipment.
Philips. (2022). CT Scanner Longevity and Software Updates.
Siemens Healthineers. (2023). Extending the Lifespan of MRI Machines.
Topol, E. (2021). Deep Medicine: How AI Can Make Healthcare Human Again.
UNEP. (2022). E-Waste Management in the Medical Sector.
Watson Health. (2022). AI and Cloud-Based Imaging Solutions.
WHO. (2023). Priority Medical Devices Initiative Report.
Have you had this concern in your facility or institution? Please share what options and or mitigation you consider viable steps to help create a collective approach to address this concern. I have seen equipment donations to Lower and Middle Income Countries. Some of these donations in form of retired equipment and devices. Is it an ethical way of dealing with the problem or dumping obsolete gadgets many of which have radioactive components?
Please share your feedback below
