Awareness Under Anesthesia: Myth or Reality?
4/6/20254 min read

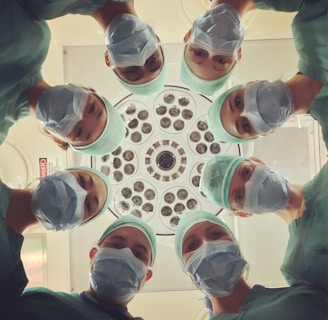
Understanding Intraoperative Awareness
Intraoperative awareness refers to the phenomenon where a patient becomes conscious during surgery while under general anesthesia. This state can involve varying degrees of sensory perception and cognitive function, ranging from vague awareness of the surroundings to full consciousness, including the ability to recall sensory experiences. Such occurrences can lead to psychologically distressing experiences and have drawn attention in the medical field.
This phenomenon is characterized by multiple types, including ‘anesthesia awareness,’ where the patient is conscious but unable to move or communicate due to muscle relaxants. The other type, known as ‘conscious awareness during anesthesia,’ can result in the patient experiencing sight, sounds, or pain but lack the ability to respond or react. It is notable that the experiences of patients who undergo intraoperative awareness can vastly differ, with some reporting feelings of fear or helplessness and others mentioning a relative lack of emotional distress.
Furthermore, patients with a history of drug abuse, those undergoing high-risk surgical procedures, or individuals with specific medical conditions may also be at an increased risk for awareness. Distinguishing between ‘awareness’ and ‘anesthesia awareness’ is crucial in understanding this phenomenon. While both terms relate to the consciousness experienced during anesthesia, ‘anesthesia awareness’ is specifically tied to the experience of being aware without the ability to interact or respond, emphasizing the complexities and implications of consciousness during surgical interventions.
The Science Behind Anesthesia and Preventative Measures
Anesthesia plays a crucial role in modern medicine, allowing for surgical procedures to be performed with minimal discomfort and anxiety for the patient. The mechanisms of anesthesia can be categorized into different types: general anesthesia induces a reversible loss of consciousness, while regional anesthesia blocks sensation in specific body areas. The specific choice of anesthetic agent depends on several factors, including the type of surgery, the patient's health status, and potential drug allergies.
The administration of anesthetic drugs is typically conducted through inhalation or intravenous routes. Inhalational anesthetics, such as nitrous oxide or sevoflurane, are delivered via a breathing mask, allowing for rapid adjustment of anesthesia levels. Intravenous anesthetics, such as propofol or thiopental, are injected directly into the bloodstream, providing quick onset of unconsciousness. Both methods facilitate comprehensive control over the depth of anesthesia, which is essential for preventing awareness under anesthesia.
Anesthesiologists employ various measures to minimize the risk of intraoperative awareness, a phenomenon where patients retain some level of consciousness while being anesthetized. Close monitoring of vital signs, including heart rate, blood pressure, and oxygen saturation, is standard practice during surgery. Additionally, anesthesia depth can be assessed using devices that measure brain activity, such as the bispectral index (BIS) monitor. These tools help anesthesiologists tailor the dosage of anesthetic agents per the patient's physiological responses, ensuring optimal sedation levels and reducing the chance of awareness.
Ensuring patient safety is paramount, and meticulous protocols are in place to assess and prepare for potential complications. Anesthesiologists perform preoperative evaluations to develop tailored anesthesia plans based on individual patient needs and risks. Such comprehensive strategies underscore the commitment of the medical community to safeguard patients' experiences during surgical interventions.
Real-life Accounts and Psychological Impact
Awareness under anesthesia has been a subject of both medical inquiry and patient testimony, particularly focusing on the phenomenon known as intraoperative awareness. Numerous case studies illustrate the distressing realities that some individuals have faced during surgical procedures. Reports tell of patients who, despite being under general anesthesia, experienced varying degrees of awareness. They could hear the conversations of medical staff or feel pain but were utterly unable to communicate or move. These harrowing experiences can range from brief moments to extended episodes, leading to significant emotional and psychological consequences following the surgery.
Patients who have undergone intraoperative awareness often recount feelings of panic and helplessness. An individual who experienced such an event during heart surgery voiced the terror of being aware of surgical activities while being completely immobilized, unable to express their distress. This trauma can have profound implications for a patient’s mental health. Many report symptoms akin to post-traumatic stress disorder (PTSD) following their encounters, which may manifest as anxiety, flashbacks, or nightmares related to the event. Research indicates that as many as 30% of individuals who experience intraoperative awareness may develop long-term psychological effects.
The impact of these experiences extends beyond individual patients, potentially influencing wider perceptions of surgical safety and trust in healthcare providers. Patients who have endured awareness under anesthesia may question the effectiveness of anesthesia practices and harbor fears regarding surgical procedures. Such concerns can deter individuals from seeking necessary medical interventions, which amplifies the importance of understanding and addressing this phenomenon. The psychological ramifications must therefore be recognized and integrated into patient care, emphasizing the need for heightened awareness and further research into intraoperative awareness to improve surgical practices and patient education.
Debunking Myths and Addressing Concerns
Awareness under anesthesia is a topic shrouded in numerous myths and misconceptions. One prevalent myth suggests that awareness during surgery is common; however, scientific evidence indicates that the incidence is rare, affecting approximately 0.1 to 0.2% of patients undergoing general anesthesia. This statistic reflects the significant advancements in anesthetic techniques and monitoring equipment, which have notably lowered the risks associated with anesthesia.
Moreover, another misconception is the belief that patients who experience awareness will remember it in a distressing manner. Research has shown that those who awaken during surgery often do not retain memories of the experience. In fact, the mind may block unpleasant sensations or memories, leading to a reduced likelihood of post-operative psychological issues. Modern anesthetic agents are designed to minimize the chances of awareness and can be adjusted according to individual patient needs, thus further enhancing safety.
With continuous advancements in anesthesia practices, the emphasis on patient safety has become paramount. Innovations such as enhanced monitoring systems and individualized anesthetic plans help ensure that patients remain adequately sedated throughout surgical procedures. Additionally, ongoing research is dedicated to improving anesthetic methods, aiming to address potential concerns and tailor approaches to specific patient profiles.
To mitigate any apprehensions surrounding anesthesia, patients are encouraged to engage in open discussions with their medical team prior to undergoing surgery. Establishing a clear line of communication allows patients to voice their fears, ask questions regarding the anesthesia process, and understand the measures taken to ensure their comfort and safety. By addressing these concerns thoughtfully, patients can feel more informed and empowered regarding their health care decisions.
