Understanding Biothesiometry: A Noninvasive Approach to Measure Vibration Perception
4/5/20254 min read
What is Biothesiometry?
Biothesiometry is a noninvasive medical test designed to assess vibration perception threshold (VPT), which is the lowest level of vibrational stimulus an individual can detect. The test primarily involves the use of a handheld vibrating device placed on the patient’s skin, typically at specific points on the extremities. By systematically varying the intensity of the vibration, clinicians can determine the threshold at which the patient perceives the vibration, thereby providing critical information about the sensory pathways involved in vibration perception.
The principles behind biothesiometry rely on the understanding of sensory nerve function and the detection mechanisms of vibration. The vibration is transmitted through the skin and sensed by specialized receptors known as mechanoreceptors. These receptors convert the external stimulus into electrical impulses that travel through the nervous system to the brain, facilitating perception. Therefore, abnormalities in VPT can serve as indicators of various underlying conditions related to the nervous system.
Biothesiometry is particularly valuable in diagnosing a range of neurological disorders, including diabetic neuropathy, peripheral neuropathy, and multiple sclerosis. For instance, diabetic patients may develop impaired nerve function due to chronic high blood sugar levels, which could be detected early through vibrational perception testing. Moreover, biothesiometry can also help in monitoring the effectiveness of treatment interventions by assessing changes in VPT over time.
This noninvasive test boasts the advantages of being safe, quick, and easy to perform, making it an ideal tool in both clinical settings and research. As a result, biothesiometry not only facilitates the early detection of neurological impairments but also plays a critical role in understanding the extent of damage and guiding therapeutic strategies. Grasping this foundational concept is essential for professionals involved in the diagnosis and management of sensory disorders.
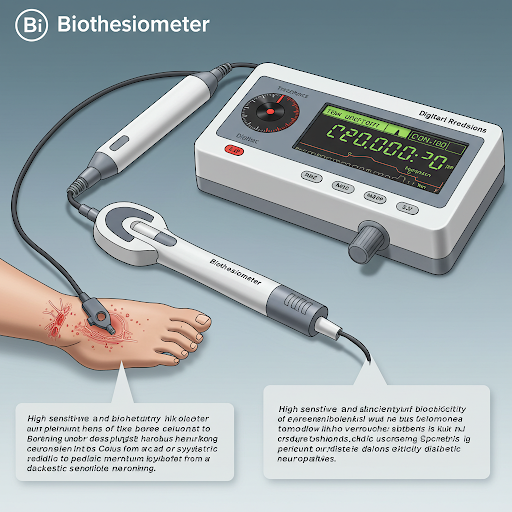
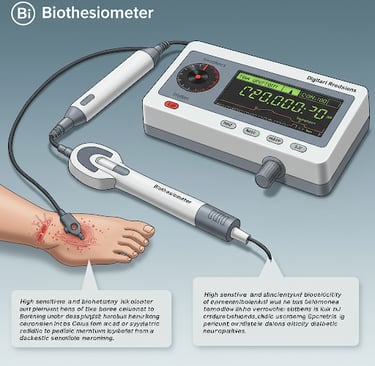
The Biothesiometer: The Tool Behind the Test
The biothesiometer is a specialized instrument designed to measure vibration perception thresholds, playing a crucial role in assessing sensory nerve function. This handheld device is pivotal in both clinical and research settings, providing reliable data on how individuals perceive vibrations. The biothesiometer typically comprises two main components: a vibrating probe and a digital display unit. The probe is applied to the area being tested, usually a fingertip or a toe, and is responsible for delivering various frequencies of vibration.
The mechanics of the biothesiometer rely on a motor that generates controlled vibrations, stimulating the sensory receptors within the skin. As the probe vibrates, the user is asked to indicate when they can feel the stimuli. The sensitivity of the device allows precise measurement of the minimum vibration the individual can detect, which is crucial for diagnosing neuropathies and other sensory disorders. Typically, the device operates at different frequencies, often ranging from 1 to 100 Hz, which enables comprehensive assessment across a spectrum of vibration perception.
In the market, several types of biothesiometers are available, varying in terms of complexity and features. While some models are simple and designed for basic assessments, others may come equipped with advanced functionalities, such as data storage and analysis capabilities. For instance, more sophisticated devices can record and analyze different parameters, allowing healthcare professionals to compare results across multiple tests over time. The display unit also plays an essential role, presenting results in a clear format that allows for immediate interpretation, assisting clinicians in making informed decisions.
Ultimately, understanding the biothesiometer’s components and functionality is integral to comprehending its significance in evaluating vibration perception. This tool not only aids in diagnosis but also enhances our understanding of sensory nerve health.
Clinical Applications of Biothesiometry
Biothesiometry, as a noninvasive method for measuring vibration perception thresholds (VPT), has emerged as a valuable tool in clinical practice, particularly in the diagnosis and management of various medical conditions. One of the most prominent applications is in the assessment of diabetic neuropathy, a complication often seen in patients with diabetes mellitus. Diabetic neuropathy can lead to diminished sensation, which increases the risk of foot ulcers and other injuries. By utilizing biothesiometry to evaluate a patient's vibration perception, healthcare practitioners can effectively identify early signs of neuropathy, allowing for timely intervention.
Additionally, biothesiometry has proven useful in assessing erectile dysfunction (ED). Research indicates that erectile dysfunction can have neurogenic origins, potentially linked to nerve damage or compromised blood circulation. By measuring VPT in the genital region, clinicians can establish a relationship between vibration sensation and sexual health, aiding in diagnosing erectile dysfunction. This method provides a quantifiable measure that contributes to understanding the severity of the condition and tailoring appropriate treatment options.
The results gleaned from biothesiometry not only assist in diagnosing these conditions but also play a significant role in staging disease progression. Higher-than-average VPT readings can indicate the advancing severity of neuropathy, prompting further investigation or changes in a patient's management plan. It is critical for practitioners to consider the correlation between VPT and various physiological parameters as part of a comprehensive diagnostic approach.
The clinical significance of biothesiometry has been reinforced by various studies demonstrating its efficacy in different medical fields, including neurology and urology. As research expands on its applications, biothesiometry may continue to evolve as a standard practice in evaluating vibration perception and contributing to evidence-based patient care.
The Future of Biothesiometry in Healthcare
Biothesiometry has emerged as a significant tool in the realm of healthcare, primarily focusing on the measurement of vibration perception thresholds. Its noninvasive nature offers distinct advantages over traditional diagnostic techniques. As we progress into a new era of technological advancements, we can anticipate several enhancements that could broaden the scope of biothesiometry applications within healthcare.
One of the prominent future directions for biothesiometry is the integration of digital technologies. Innovations such as wearable devices equipped with biothesiometry sensors could enable continuous monitoring of vibration perception in patients. This advancement could facilitate early detection of neuropathies and diabetes-related complications, thus leading to timely interventions. Additionally, incorporating artificial intelligence into biothesiometry could enhance the accuracy of assessments, allowing healthcare professionals to better predict patient outcomes based on individual vibration thresholds.
Furthermore, research into the application of biothesiometry across different medical fields is likely to expand. For instance, its potential role in neurology could be profound, particularly in assessing conditions like multiple sclerosis or Parkinson's disease where sensory processing is affected. The ability to measure vibration perception may provide critical insights into the progression of such illnesses and aid in the formulation of tailored therapeutic strategies.
Continued research is vital to ascertain the most effective uses of biothesiometry. Collaboration among researchers, clinicians, and device manufacturers will be essential to establish standardized protocols for the measurement and interpretation of vibration perception thresholds. As more healthcare stakeholders recognize the importance of this noninvasive diagnostic tool, we can expect enhanced support for research initiatives aimed at improving care through better understanding of vibration perception.
In conclusion, biothesiometry holds considerable promise for the future of healthcare. With ongoing innovations, expanded applications, and a focus on research, this noninvasive approach to measuring vibration perception is poised to significantly influence patient care and outcomes in the years to come.
