Understanding Bioartificial Liver Devices: A Novel Approach to Liver Failure Treatment
4/3/20258 min read
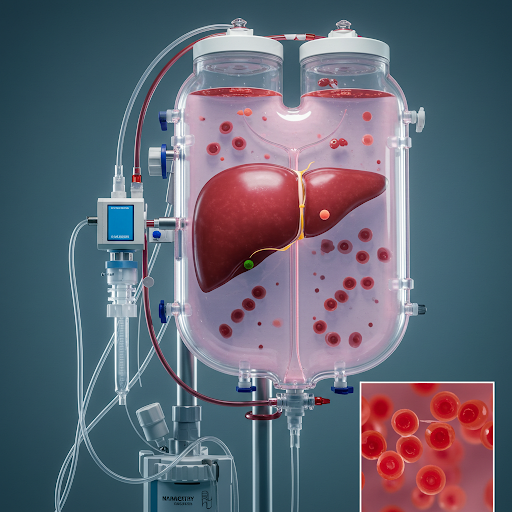
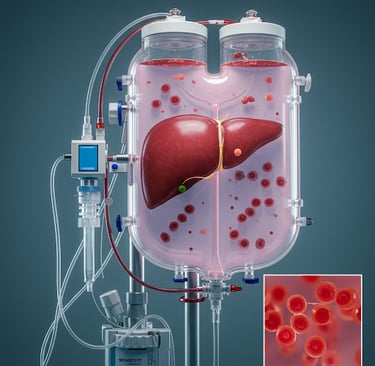
Introduction to Bioartificial Liver Devices
Bioartificial liver devices (BALs) represent an innovative approach in the management of liver failure, addressing a significant gap in current medical treatments for patients with compromised hepatic function. These devices serve a dual purpose: they not only assist in maintaining vital metabolic functions associated with the liver but also provide a patient with temporary support while awaiting transplantation or potential recovery of liver function. The significance of BALs lies in their potential to bridge the gap between medical management and the need for a liver transplant, which remains a strict and often time-consuming option for many patients suffering from acute or chronic liver disease.
The underlying principle of bioartificial liver devices is to mimic the biological functions of a healthy liver, utilizing both artificial components and biological materials. Typically, BALs utilize porcine liver cells or other engineered cells to perform essential functions such as detoxifying blood, producing proteins, and modulating nutrients. The combination of biological and mechanical components allows BALs to enhance the biochemical processes inherent within the liver, effectively supporting the patient during critical episodes of liver failure. This innovative technology is crucial in hepatology, as it helps stabilize patients who might otherwise face dire consequences without immediate intervention.
Furthermore, the application of BALs extends to diverse forms of liver dysfunction, providing a customizable approach to treatment based on individual patient needs. Modern advancements in materials science and cell engineering have spurred research, leading to enhanced designs of these devices, striving for improved biocompatibility and functionality. As the field of hepatology evolves, understanding the role and mechanics of bioartificial liver devices will be crucial for healthcare professionals tasked with diagnosing and managing liver-related disorders. The exploration of BALs continues to illustrate their potential impact on improving patient outcomes in liver failure scenarios.
Mechanism of Action of Bioartificial Liver Devices
Bioartificial liver devices (BALs) represent a significant advancement in the treatment of acute and chronic liver failure by mimicking essential functions of the liver. The core mechanism of action lies in their ability to detoxify blood and provide synthetic support, mitigating the effects of liver dysfunction. These devices typically employ living cell lines, such as hepatocytes, which are derived from either animal or human sources, to replicate the metabolic processes of a healthy liver.
Detoxification is one of the primary functions performed by bioartificial liver devices. The patient’s blood is circulated through the device, where hepatocytes work to filter and eliminate various toxins and metabolic waste products. These toxins can result from the body's own metabolic processes, as well as exogenous substances like drugs and alcohol. By leveraging the enzymatic activities of the living cells, BALs can effectively perform gluconeogenesis, urea synthesis, and ketogenesis, which are critical for maintaining metabolic homeostasis.
Additionally, BALs serve to provide synthetic support to patients with liver failure by supplying essential proteins and maintaining albumin levels. The hepatocytes within the device can synthesise important proteins, including clotting factors and albumin, which are often deficient in individuals suffering from liver disease. This not only helps in normalizing blood coagulation but also assists in maintaining oncotic pressure and fluid balance within the body.
The effectiveness of bioartificial liver devices has been an area of active research, with ongoing studies focusing on enhancing the viability and function of the hepatocyte populations used. Various parameters, such as culture conditions and bioreactor design, continue to be optimized to ensure that these living cell lines retain their functionality over extended periods. As a result, BALs hold the promise of improving patient outcomes by providing a functional bridge to liver transplantation or aiding the recovery of the hepatic system in patients facing acute liver conditions.
Types of Bioartificial Liver Devices
Bioartificial liver devices (BALs) represent a significant advancement in the treatment of liver failure, offering alternatives to liver transplantation. Among the myriad of systems available, two primary types stand out: the HepatAssist 2000 and the ELAD (Extracorporeal Liver Assist Device) system. These devices not only serve to temporarily support liver function but also exhibit unique methodologies regarding cellular composition and functionality.
The HepatAssist 2000 utilizes porcine hepatocytes, which are pig liver cells, to facilitate metabolic functions. This device aims to provide patients with a biological substitute for a failing liver, effectively performing critical tasks such as detoxification and albumin production. The use of porcine cells is particularly noteworthy, as they possess similar physiological properties to human hepatocytes, allowing for effective metabolic processing. In some clinical trials, the HepatAssist 2000 has shown promise in improving patient outcomes, specifically for those awaiting a liver transplant, by maintaining essential liver functions over a sustained period.
Conversely, the ELAD system employs human hepatoblastoma C3A cell lines, a type of immortalized cell that retains specific liver functions. These cell lines are derived from human liver tissue and are modified to survive outside the body. The ELAD system is designed to simulate the in vivo environment of a healthy liver, providing essential metabolic and synthetic activities. This differentiation is crucial, as the use of human cells minimizes the risk of immune rejection, which can complicate therapy. The ability of the ELAD system to adjust to the biochemical requirements of the patient further enhances its therapeutic potential.
In summary, both the HepatAssist 2000 and the ELAD system illustrate the promise of bioartificial liver devices in managing liver failure. Their distinct approaches—utilizing porcine hepatocytes and human C3A cell lines—underscore the versatility and ongoing innovation within the field of liver support technologies.
Clinical Applications and Trials
Bioartificial liver devices (BALDs) have emerged as promising therapeutic options for patients suffering from acute or chronic liver failure. These innovative systems integrate biological and artificial components to take over the liver's metabolic, synthetic, and detoxification functions. Their primary clinical application is to provide temporary support for patients awaiting liver transplantation or as a bridge-to-transplantation strategy. This approach aims to stabilize patient conditions, allowing time for regeneration of native liver functions or for suitable donor organs to become available.
Several clinical trials have explored the efficacy and safety of BALDs in various settings. For instance, a notable study assessed the use of the extracorporeal liver assist device (ELAD) in patients with acute liver failure. The trial indicated a significant reduction in bilirubin levels after treatment, suggesting potential for improved patient outcomes. Furthermore, the use of BALDs has expanded to include patients with hepatotoxic drug overdoses, where the device serves as a critical intervention to mitigate liver damage and improve overall survival rates.
Ongoing clinical trials are investigating different configurations of bioartificial liver systems, including those that utilize hepatocyte cultures or stem cell-derived hepatocytes to enhance performance. Results from these investigations show promising trends, with many patients demonstrating temporary improvement in liver function as evidenced by biochemical and clinical markers. Additionally, researchers are assessing the long-term impacts of BALDs, which may include not only immediate liver support but also improvements in overall organ recovery.
In conclusion, bioartificial liver devices represent a potentially transformative technology for managing liver failure. With ongoing clinical trials aimed at refining these systems and validating their effectiveness, there is a hopeful outlook for improving patient care in this critical area of medicine.
Advantages of Bioartificial Liver Devices
Bioartificial liver devices present a groundbreaking advancement in the treatment options for patients suffering from liver failure. One primary advantage of these devices is their potential to significantly improve the quality of life for patients by providing a temporary solution that mimics the functions of a healthy liver. This capability allows patients to experience a reduction in symptoms associated with hepatic insufficiency, such as jaundice, fatigue, and coagulopathy, thus enhancing their overall well-being during a critical period.
Moreover, bioartificial liver devices can contribute to increased survival rates among individuals awaiting liver transplantation. By supporting hepatic function temporarily, these devices afford patients a crucial window of time to stabilize while waiting for a suitable donor organ. This bridging role is particularly vital given the current shortage of available donor livers, making bioartificial liver devices an invaluable resource in the management of acute liver failure and chronic liver diseases.
In addition to their immediate medical benefits, bioartificial liver devices also create new prospects for liver transplantation. They can serve as a bridge to recovery for patients with acute liver injury, allowing the liver to potentially heal on its own. In scenarios where spontaneous recovery is unlikely, these devices can facilitate a patient’s transition to transplantation by maintaining homeostasis and organ function until a donor can be identified. This functionality not only increases the likelihood of a successful transplant but also helps to ensure that patients are in optimal condition to receive a new liver.
In summary, the advantages of bioartificial liver devices extend from enhancing patient quality of life to potentially increasing survival rates and improving outcomes related to liver transplantation. Their role as a supportive therapy during critical times underscores their importance in the contemporary management of liver diseases.
Challenges and Limitations
Bioartificial liver devices (BALDs) have emerged as a promising approach to addressing liver failure; however, they are not without challenges and limitations that hinder their widespread use in clinical practice. One significant technical hurdle lies in the complexity of replicating liver functions that are inherently multifaceted. The liver is responsible for a variety of metabolic and synthetic processes, including detoxification, protein synthesis, and the regulation of biochemical substances. To effectively replace these functions, BALDs must integrate advanced cell culture techniques with biocompatible materials while maintaining viability and functionality of hepatocytes. Failure to achieve this may result in suboptimal clinical outcomes, thereby limiting the efficacy of such devices.
Furthermore, regulatory issues pose another critical challenge for the development and application of BALDs. The pathway to obtaining regulatory approval involves rigorous testing to demonstrate safety and efficacy. This includes preclinical studies followed by extensive clinical trials, which can be both time-consuming and costly. The unpredictable nature of regulatory demands may dissuade researchers and manufacturers from pursuing BALD technologies, thus stalling innovation and limiting patient access to these potentially life-saving devices.
Additionally, biological considerations complicate the use of bioartificial liver devices. The incorporation of living cells, particularly human hepatocytes, presents risks such as cellular rejection and immunogenic responses. Moreover, the variability in liver functionality among patients due to underlying health conditions can lead to inconsistent results when utilizing BALDs. These biological challenges necessitate further research to enhance the integration of BALDs with the human body and ensure patient-specific adaptability.
Future Prospects of Bioartificial Liver Technology
The landscape of bioartificial liver technology is rapidly evolving, potentially redefining treatment methodologies for liver failure. Recent advancements in cellular engineering, biomaterials, and computational modeling highlight a promising trajectory for these devices, setting the stage for significant improvements in patient outcomes. One area of notable exploration involves the enhancement of hepatocyte function through genetic engineering. Researchers are investigating methods to increase the viability and efficiency of hepatocytes within bioartificial liver systems. This includes the modulation of metabolic pathways to enhance the detoxification capabilities of the cells, promising a more effective therapeutic approach for liver disease.
Furthermore, the integration of artificial intelligence and machine learning algorithms is expected to enhance the functionality of bioartificial liver devices. By utilizing data-driven insights, customized treatment regimens can be developed, allowing for personalized patient care. These advancements could lead to real-time monitoring of liver function and tailored interventions, thereby optimizing patient responses to treatment. This adaptability aligns with the growing trend towards precision medicine, where individual variations are accounted for in therapeutic applications.
Another vital prospect lies in the scalability and accessibility of bioartificial liver devices. As research continues, efforts are being made to develop cost-effective manufacturing processes that would allow broader access to these innovative treatments. Enhanced scalability could lead to widespread use in clinical settings, addressing the urgent need for effective liver support systems, especially in regions with high incidence rates of liver diseases.
In conclusion, the future of bioartificial liver technology rests on a foundation of continuous research and innovation. The focus on advanced cellular technologies, integration of AI, and cost-effective solutions showcases the industry's commitment to addressing liver failure comprehensively. As these advancements unfold, they hold the potential to transform the existing paradigms of liver treatment, offering hope to countless patients worldwide.
