Evaluating the ROI of Health Management Systems: A Comprehensive Guide
Implementing a health management system (HMS) involves understanding initial investments for software acquisition and ongoing expenses. Learn how to effectively budget for your HMS to ensure successful implementation and management.
9/28/20258 min read


Introduction to Health Management Systems
The landscape of healthcare has undergone significant transformations over the past few decades, paving the way for the emergence of Health Management Systems (HMS). Originally considered optional digital tools, these systems have evolved into essential core infrastructures within various healthcare settings, including hospitals, clinics, and small practices. This evolution reflects a broader trend toward digitization and the increasing recognition of data-driven approaches in healthcare delivery.
Health Management Systems encompass a variety of functionalities that aim to streamline operations and improve patient care. At their core, these systems facilitate the organization, storage, and analysis of health data, allowing healthcare providers to make informed decisions that enhance the quality of care they deliver. The integration of HMS into healthcare practices aids in managing patient records, scheduling appointments, and tracking treatment outcomes, making them indispensable for modern healthcare operations.
Moreover, HMS are critical for enhancing patient engagement and supporting communication between providers and patients. The availability of patient portals and telehealth options within these systems empowers individuals to take an active role in their health management, ultimately leading to improved health outcomes. Furthermore, these systems contribute to significant operational efficiencies, reducing administrative burdens and minimizing errors associated with traditional record-keeping methods.
As healthcare organizations strive to enhance their services while maintaining profitability, understanding the return on investment (ROI) of Health Management Systems becomes paramount. Evaluating the financial benefits related to the adoption of HMS is essential not only for justifying the initial investment but also for ensuring sustainable growth within the industry. This blog post will delve deeper into the various aspects of HMS, offering insights into their impact and the significance of assessing their ROI.
Understanding Costs: Initial Investment and Ongoing Expenses
Implementing a health management system (HMS) necessitates a comprehensive understanding of the associated costs, which can be broadly categorized into initial investments and ongoing expenses. The initial investment represents the upfront financial commitment required for software acquisition, hardware upgrades, and system integration. This stage is crucial as it lays the foundation for the effective functioning of the HMS and typically involves a significant allocation of resources.
The software acquisition cost depends largely on the type and capabilities of the chosen health management system. Options may range from off-the-shelf software solutions to customized platforms designed specifically to meet the unique needs of a healthcare organization. It is imperative for decision-makers to evaluate the features and functionalities these systems provide against their operational requirements to ensure an appropriate investment.
In addition to software, hardware upgrades may be indispensable depending on the existing infrastructure. This can involve purchasing new servers, additional storage, or enhanced networking equipment for optimal system performance. Furthermore, system integration services, which ensure that the HMS effectively communicates with other operational systems, should also be factored into the initial investment costs.
Once the setup is complete, ongoing expenses must be accounted for to maintain system efficiency and effectiveness. These expenses encompass regular maintenance, software updates, and necessary system upgrades to adapt to evolving healthcare standards and technologies. Training for staff is another essential cost element, as it ensures that personnel are proficient in utilizing the HMS, thereby maximizing the system's benefits. Lastly, organizations may incur subscription fees for cloud-based solutions, which must be considered in the total cost of ownership.
By analyzing both the initial investment and ongoing expenses in detail, healthcare organizations can accurately assess the financial commitment required to implement an efficient health management system, thereby enhancing their decision-making process.
Direct Benefits of Health Management Systems
Health Management Systems (HMS) offer a variety of direct benefits to healthcare providers, significantly enhancing operational efficiency and patient care. One of the most notable advantages is the improvement in billing accuracy. By automating billing processes and reducing manual errors, HMS minimizes the occurrence of discrepancies and thus leads to faster reimbursements. Accurate invoices facilitate clearer communication with patients regarding their financial responsibilities, ultimately enhancing revenue cycle management.
Another crucial benefit is the streamlined patient registration process. Traditional registration methods often involve lengthy paperwork, consuming valuable time for both patients and administrative staff. With HMS, patient data can be captured electronically, allowing for quicker check-ins and minimizing waiting times. This efficiency not only improves patient satisfaction but also frees up staff to focus on more critical tasks within the healthcare facility.
Enhanced appointment scheduling represents yet another advantage of utilizing health management systems. These systems allow for automated appointment reminders and easy rescheduling options, reducing no-show rates significantly. By optimizing appointment slots, healthcare providers can maximize their resources and improve patient throughput. This efficiency directly translates into better utilization of clinical staff and facilities, leading to substantial productivity gains.
Furthermore, effective inventory management is imperative in a healthcare setting. Health management systems provide real-time tracking of medical supplies and equipment, helping institutions maintain optimal stock levels. This proactive approach not only minimizes waste but also ensures that essential items are readily available when needed, ultimately enhancing overall patient care. With improved inventory oversight, healthcare providers can achieve significant cost savings while also improving the quality of care delivered.
Overall, the direct benefits of implementing a health management system significantly contribute to enhanced operational effectiveness and improved patient experiences in healthcare facilities.
Indirect Benefits: Enhancing Patient Outcomes and Experience
Health management systems play a pivotal role in transforming the ways healthcare providers interact with patients, thus leading to enhanced patient outcomes and experiences. One of the primary indirect benefits of these systems is improved data management. By facilitating the organization and accessibility of health records, these systems enable the delivery of personalized care that considers the unique medical history, preferences, and needs of each patient. This tailored approach not only increases satisfaction but also promotes better health outcomes.
Furthermore, the implementation of health management systems can significantly reduce medication errors, a common issue that adversely affects patient safety. Accurate prescription management, reminders for medication refills, and alerts for potential drug interactions are just a few functionalities these systems provide. By minimizing such errors, health management systems contribute to optimal treatment regimens, thereby fostering a more positive patient experience and encouraging adherence to prescribed therapies.
Engagement is another key aspect enhanced by health management systems. Patient portals allow individuals to access their health information, schedule appointments, and communicate directly with their healthcare providers, fostering a sense of ownership over their healthcare journey. This elevated level of interaction promotes patient engagement, leading to higher satisfaction rates. Moreover, when patients feel actively involved in their care, they are more likely to retain information about their treatment plans and exhibit better health management practices.
Effective communication between providers and patients is also enhanced through health management systems. Secure messaging features and shared care plans ensure that both parties are aligned, which is essential for continuous care. Ultimately, these factors collectively influence retention rates and referral patterns, as satisfied patients are more likely to recommend healthcare providers to family and friends. In conclusion, the indirect benefits of health management systems significantly contribute to a more effective and personalized healthcare experience, reinforcing the value of such investments in the medical field.
Calculating the ROI: Metrics and Methods
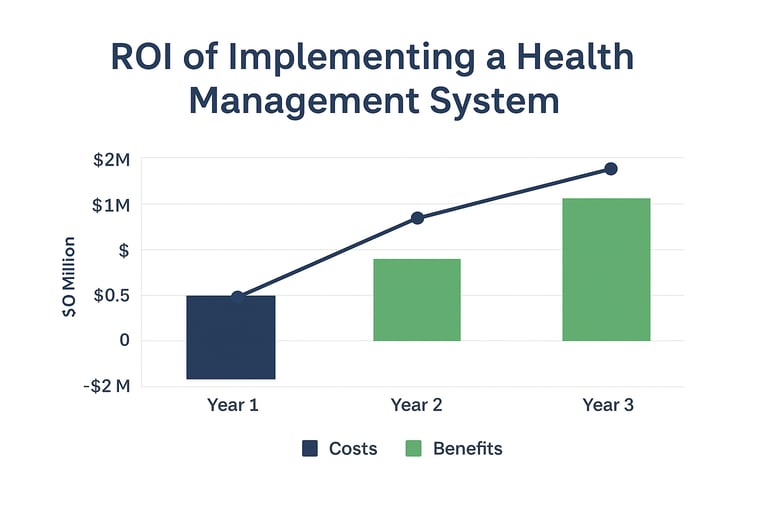
Calculating the return on investment (ROI) for health management systems involves a comprehensive assessment of both financial and non-financial metrics. Healthcare administrators can employ various methods to evaluate their investments effectively. One significant approach includes determining the payback period, which is the time it takes for an organization to recover its initial investment from the net cash flows generated by the system. This metric is crucial in understanding the timeframe within which a system becomes financially viable.
Another essential metric is the net present value (NPV), which takes future cash flows expected from the health management system and discounts them back to their present value. This approach allows administrators to account for the time value of money and assess whether the projected benefits outweigh the initial costs. An NPV greater than zero indicates that the investment will yield positive returns over time.
Return on investment (ROI) percentage is yet another useful metric. This calculation provides a straightforward way to measure the efficiency of the investment. The formula for calculating ROI is relatively simple: subtract the total cost of the investment from the total return, and then divide the result by the total cost. This percentage helps to convey how much profit is gained for each dollar spent on the health management system.
It is also important to consider non-financial returns when calculating ROI. Metrics such as improvements in patient outcomes, enhanced operational efficiency, and increased staff satisfaction can significantly impact the overall effectiveness of a health management system. By incorporating both financial and non-financial returns into the evaluation process, healthcare administrators can develop a holistic view of the value created by these systems, thus making more informed financial decisions tailored to their specific healthcare environments.
Case Studies: Successful HMS Implementation and ROI Realization
Health Management Systems (HMS) have been adopted across various healthcare facilities, demonstrating diverse implementations that yield significant returns on investment (ROI). This section highlights case studies from different sectors, reflecting the challenges faced and the resultant benefits achieved through HMS integration.
One notable case study is the implementation of an HMS in a regional hospital that was grappling with inefficient patient record-keeping and lengthy discharge processes. By integrating an electronic health record (EHR) component within the HMS, the hospital was able to streamline its operations. This transition not only minimized the average time spent on patient documentation but also enhanced data accessibility for healthcare providers. Following the implementation, the hospital reported a 25% reduction in discharge times and a 35% increase in patient satisfaction scores, leading to a measurable ROI within the first year of operation.
Another compelling example comes from a small community clinic that sought to improve patient engagement and chronic disease management. By adopting a comprehensive HMS that included telehealth services and patient management tools, the clinic successfully increased patient participation in care programs. The clinic recorded a significant rise in follow-up appointments, which contributed to a decrease in hospital readmission rates by 15%. The financial savings from fewer hospitalizations, coupled with the increased revenue from more engaged patients, positioned the clinic to realize an impressive ROI shortly after implementation.
Lastly, a large urban university hospital faced significant challenges with interdepartmental communication and coordination of care. The implementation of a robust HMS facilitated real-time data sharing among departments. This resulted in improved clinical decision-making, reduced duplication of tests, and optimized resource utilization. Subsequently, the hospital achieved a 20% decrease in operational costs, showcasing the financial advantages of effective HMS deployment.
These case studies exemplify how diverse healthcare settings successfully navigate their unique challenges through HMS implementation, ultimately realizing substantial ROI. Such examples serve as practical references for decision-makers contemplating similar integration within their organizations.
Conclusion: Strategic Decision-Making for Health Management System Adoption
In the evolving landscape of healthcare, the adoption of Health Management Systems (HMS) presents a critical opportunity for organizations to enhance operational efficiencies and improve patient outcomes. Throughout this guide, we have explored the multifaceted nature of evaluating the return on investment (ROI) associated with health management systems. It is imperative for administrators and decision-makers to understand that the implications of implementing an HMS transcend the initial financial commitment. While upfront costs are an important consideration, the analysis should encompass both direct and indirect benefits that these systems can provide over time.
Direct benefits may include improved data accessibility and streamlined workflows, leading to enhanced productivity among healthcare professionals. Conversely, indirect advantages can manifest through improved patient engagement, increased satisfaction, and better health management outcomes. These outcomes contribute significantly to the overall operational efficiency of healthcare facilities, positioning them to deliver higher standards of care and drive positive patient experiences. Addressing these broader impacts ultimately supports the case for investment in advanced health management technologies.
Moreover, as healthcare organizations strive to align their strategies with overarching goals such as quality improvement and patient-centered care, a systematic approach to the implementation of health management systems becomes vital. Decision-makers are encouraged to consider metrics that reflect long-term gains rather than solely focusing on immediate financial returns. Doing so will facilitate informed choices that not only benefit today’s operations but also pave the way for sustainable growth and adaptability in the future.
To summarize, the thoughtful adoption of health management systems should be viewed as a strategic decision that integrates financial evaluation with a holistic understanding of their potential long-term impact. Institutions that embrace this perspective will likely be better equipped to meet the demands of modern healthcare delivery effectively.