Understanding the Bair Hugger System: Maintaining Core Body Temperature in Surgical Settings
3/26/20257 min read

Introduction to the Bair Hugger System
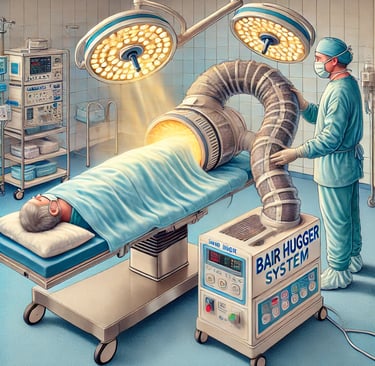
The Bair Hugger System is a medical device primarily designed for the management of a patient’s core body temperature in surgical and clinical settings. Maintaining an appropriate body temperature during procedures is crucial, as hypothermia can lead to various complications, such as increased risk of infections, prolonged recovery times, and impaired coagulation. The Bair Hugger employs a innovative convective warming technique that helps to prevent these adverse outcomes by ensuring that patients are kept warm throughout their surgical experience.
This system consists of a warming unit that blows warm air into a specialized blanket or gown that envelops the patient. As the warm air circulates, it gently warms the surface of the patient’s skin, which in turn helps to maintain and stabilize their internal body temperature. The device is versatile and can be used in different surgical settings, including orthopedic, cardiac, and general surgeries, making it a valuable tool for healthcare professionals.
The importance of the Bair Hugger System in healthcare cannot be overstated. It addresses the critical need for temperature management during surgery, ultimately enhancing patient safety and comfort. Studies have shown that patients who maintain normothermia experience fewer complications post-surgery, leading to better overall outcomes and shorter hospital stays. Healthcare institutions are increasingly recognizing the role of the Bair Hugger in promoting effective thermal regulation, which is why this technology continues to be a trusted solution in surgical settings. By ensuring patients remain warm during their operations, the Bair Hugger System plays a vital role in improving surgical care and outcomes.
Historical Background and Development
The Bair Hugger System emerged in 1987 as a groundbreaking solution aimed at maintaining core body temperature in surgical settings. The initial design was conceived by Dr. Scott Augustine, who recognized the critical importance of thermal regulation during surgical procedures. Prior to the development of the Bair Hugger, methods such as forced air warming were either inefficient or uncomfortable for patients, leading to a heightened risk of hypothermia in the operating room.
The Bair Hugger System utilizes a simple yet effective approach by circulating warmed air through a disposable blanket that envelops the patient. This innovation not only helps maintain a stable body temperature but also enhances patient comfort, contributing to better surgical outcomes. Since its launch, the technology has seen continuous evolution to keep pace with advancements in medical science and the increasing demands of surgical safety.
Over the years, the system has undergone several updates aimed at improving its efficiency, safety, and user-friendliness. These advancements have included changes in the design of the warming blankets, which are now lighter and more versatile, ensuring improved coverage without compromising mobility. Additionally, the system has incorporated modern materials and technology to maximize its effectiveness while addressing concerns around air quality in the operating room.
Moreover, the Bair Hugger System has adapted to meet various standards and regulations imposed by health authorities and medical boards. Studies and clinical trials have substantiated its effectiveness in reducing perioperative hypothermia and its associated complications. As a result, the Bair Hugger has become an established and essential tool in contemporary surgical practices, consistent with the ongoing emphasis on patient safety and comfort in modern healthcare environments.
Components of the Bair Hugger System
The Bair Hugger System is a sophisticated yet straightforward thermal management solution utilized in surgical settings to maintain patients’ core body temperature. At the heart of the system are two essential components: the reusable warming unit and the single-use disposable warming blankets. Each part plays a crucial role in achieving optimal thermal regulation during surgical procedures.
The reusable warming unit is a key player in the Bair Hugger System. This device generates and circulates warm air through a network of hoses that connect to disposable blankets placed over or under the patient. Its design allows for precise temperature control, which is vital in ensuring that patients remain normothermic during surgery. The warming unit houses all necessary controls, including settings for temperature and airflow, enabling healthcare providers to customize the warming experience according to individual patient needs. This customization is vital in avoiding hypothermia, which can lead to increased surgical complications and prolonged recovery times.
Complementing the warming unit are the single-use disposable warming blankets. These blankets are designed with a unique fabric that allows warm air to be evenly distributed across the patient's body, enhancing overall warmth and comfort. The disposable aspect of these blankets ensures that they are sanitary and free from contamination between patients, thus upholding stringent infection control protocols. The lightweight and flexible nature of these blankets allows for seamless application in various surgical scenarios without hindering the surgical team’s access to the patient.
In summary, the effectiveness of the Bair Hugger System in managing core body temperature during surgery relies significantly on its two main components—the reusable warming unit and the disposable warming blankets. Together, they work harmoniously to create a controlled thermal environment that benefits patient safety and surgical outcomes.
Mechanism of Action and Operation
The Bair Hugger System is a sophisticated patient warming device designed to maintain a stable core body temperature during surgical procedures. The effectiveness of this system lies in its fundamental principles of convective heating, which involves the transfer of heat through the movement of warm air. At the core of the Bair Hugger’s operation are specially designed blankets that serve as conduits for this heated air, enveloping the patient and providing a controlled thermal environment.
The device consists of a heating unit that warms ambient air and then directs this air into a series of blankets that are draped over the patient. These blankets, often made from soft, breathable materials, feature strategically designed slots or channels to ensure even distribution of warm air. As the heated air circulates throughout the blanket, it creates a gentle warming effect, effectively raising the patient's core temperature without causing discomfort. This process is particularly advantageous because it mitigates the risk of hypothermia, which can lead to various complications during and after surgery.
Temperature management is a critical aspect of perioperative care. Maintaining normothermia before, during, and after surgical procedures improves patient outcomes significantly. It reduces the risk of surgical site infections, minimizes blood loss, and facilitates faster recovery, thereby enhancing overall patient satisfaction. Furthermore, by utilizing the Bair Hugger System, surgical teams can provide consistent and effective thermoregulation, ensuring that patients remain warm and safe throughout the entire surgical experience.
In summary, the Bair Hugger System operates through efficient convective heating, utilizing temperature management strategies that are essential for optimizing patient outcomes in surgical settings.
Clinical Applications and Benefits
The Bair Hugger System has emerged as a pivotal device in surgical settings, particularly in maintaining a stable core body temperature during various procedures. One of the primary clinical applications of this system is its role in preventing hypothermia, which can occur when patients are subjected to anesthetic agents and the cooling effects of surgical environments. The Bair Hugger System utilizes forced-air warming blankets that envelop the patient, providing a consistent and controllable warmth. This intervention is critical, as maintaining normothermia not only supports a patient's comfort but also plays a significant role in their physiological stability during surgery.
Moreover, the Bair Hugger System contributes to reducing infection rates in surgical patients. Hypothermia is known to impair immune function, ultimately leading to a heightened risk of postoperative infections. By promoting normothermia, the device enhances the overall immune response, thereby minimizing the chances of surgical site infections (SSIs). Clinical studies have indicated that patients who maintain a stable body temperature throughout the surgical process exhibit lower incidences of SSIs, which is crucial for improved patient outcomes.
Another significant benefit associated with the Bair Hugger System is its influence on healing and recovery. Maintaining a stable body temperature has been connected with optimal metabolic functioning and enhanced tissue perfusion. Consequently, patients are likely to experience reduced recovery times post-surgery. Additionally, keeping patients comfortable during surgery can lead to lower levels of intraoperative stress, ultimately promoting a more positive surgical experience for both patients and surgical teams.
In summary, the Bair Hugger System presents multiple clinical applications and benefits in surgical environments, encompassing the prevention of hypothermia, the reduction of infection risk, and the overall enhancement of patient outcomes. Its integration into surgical protocols underscores its importance in modern healthcare practices.
Safety and Regulatory Considerations
The Bair Hugger System, designed to maintain a patient’s core body temperature during surgical procedures, operates under strict safety and regulatory measures. The United States Food and Drug Administration (FDA) plays a crucial role in the approval and oversight of such medical devices. The Bair Hugger, manufactured by 3M, was cleared by the FDA for use in various surgical environments, showcasing its compliance with established safety standards. The company's adherence to these guidelines ensures that the device is both effective and safe for patients.
Hospitals and surgical centers are required to implement the Bair Hugger System according to recommended guidelines to mitigate risks. These guidelines encompass proper placement of the blanket, appropriate temperature settings, and monitoring of the patient during use. It is essential that healthcare professionals are adequately trained to utilize the Bair Hugger effectively. This knowledge allows for better decision-making regarding patient positioning and monitoring, thus minimizing potential complications.
Despite these safety measures, improper usage of the Bair Hugger can lead to complications. Potential risks include burns from excessive heat or, in rare instances, nosocomial infections that may arise from contaminants. However, research has generally shown the Bair Hugger to be a safe option when used appropriately. Regular audits and patient monitoring help ensure that safety protocols are followed, thereby enhancing the efficacy of maintaining normothermia during surgery.
In conclusion, adhering to safety and regulatory standards is paramount to the effective use of the Bair Hugger System. By understanding the FDA's role and implementing appropriate guidelines, healthcare institutions can significantly minimize risks and ensure patient safety while utilizing this essential device in surgical settings.
Future Innovations and Research
The landscape of temperature management during surgical procedures is continually evolving, and the Bair Hugger System stands at the forefront of these developments. As healthcare professionals recognize the significance of maintaining normothermia in patients, ongoing research and innovation are expected to enhance the efficacy and functionality of the Bair Hugger System. Future advancements could include the integration of smart technology, allowing for real-time monitoring and automated adjustments to a patient's temperature based on individual physiological responses.
One area of potential innovation is the incorporation of artificial intelligence (AI) and machine learning algorithms into the Bair Hugger System. Such integration may allow the system to analyze patient data more effectively, predicting temperature fluctuations and optimizing warming protocols tailored specifically to individual surgical profiles. This would greatly enhance the system's adaptability and may further minimize the risks associated with hypothermia during operations.
Research efforts are also focusing on the development of new materials and designs for warming blankets and components of the Bair Hugger System. Innovations in fabric technology could lead to lighter and more breathable materials without compromising thermal efficiency. Additionally, studies aimed at understanding the long-term outcomes related to temperature management will be pivotal in shaping clinical guidelines and best practices.
Collaboration among surgical teams, biomedical engineers, and researchers is vital for fostering these transformations. Continuous investment in studies examining the impact of the Bair Hugger System on surgical outcomes will provide evidence to support its further use and modification. As new insights and feedback emerge from the medical community, enhancements to the system's design and function are anticipated to significantly improve patient safety and comfort, thereby solidifying the role of effective temperature management in surgical settings.
