A Comprehensive Guide to Artificial Urinary Sphincters: Options, Brands, and Usage
3/22/20254 min read
Introduction to Artificial Urinary Sphincters
Artificial urinary sphincters (AUS) represent a significant advancement in the management of urinary incontinence, particularly for individuals experiencing stress urinary incontinence due to prostate surgery, neurological conditions, or other anatomical factors affecting bladder control. The primary purpose of an artificial urinary sphincter is to provide a reliable closure mechanism for the urinary bladder, ultimately improving the quality of life for those affected by involuntary leakage.
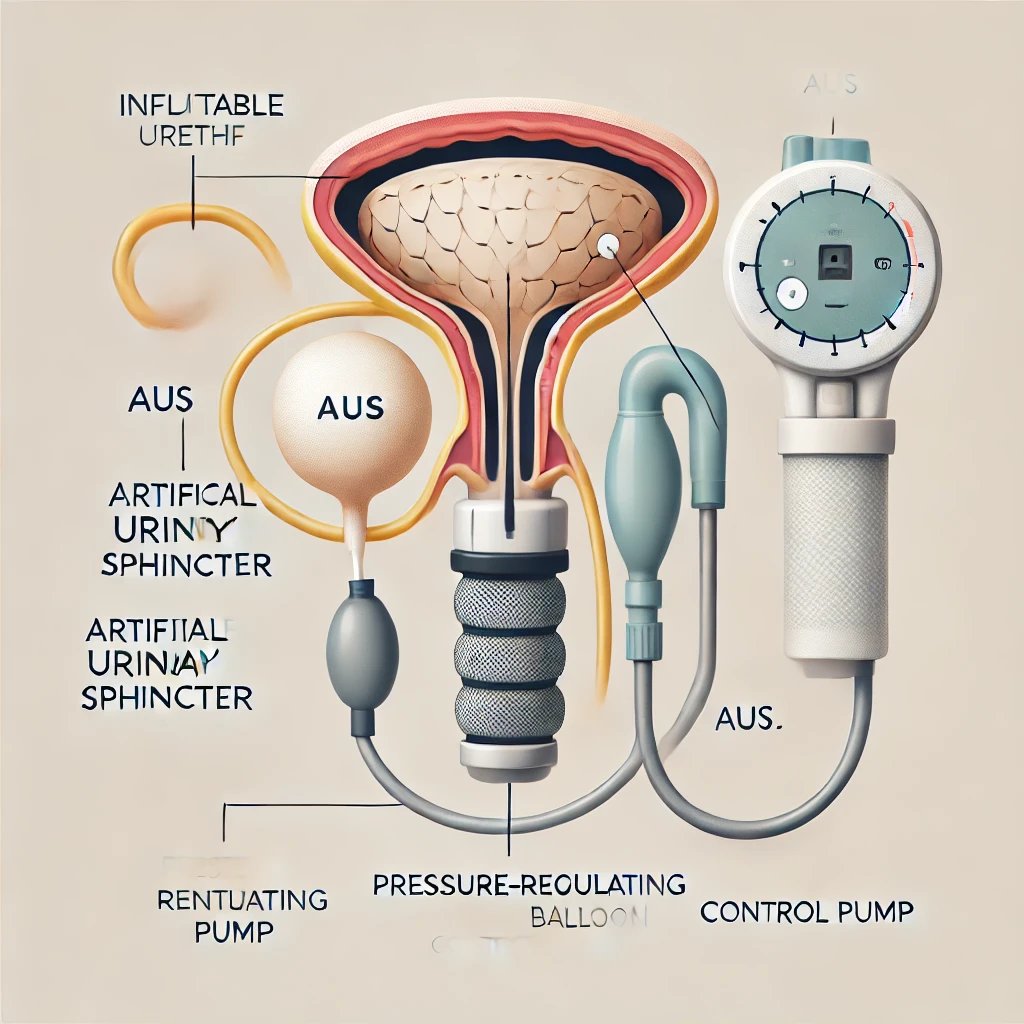
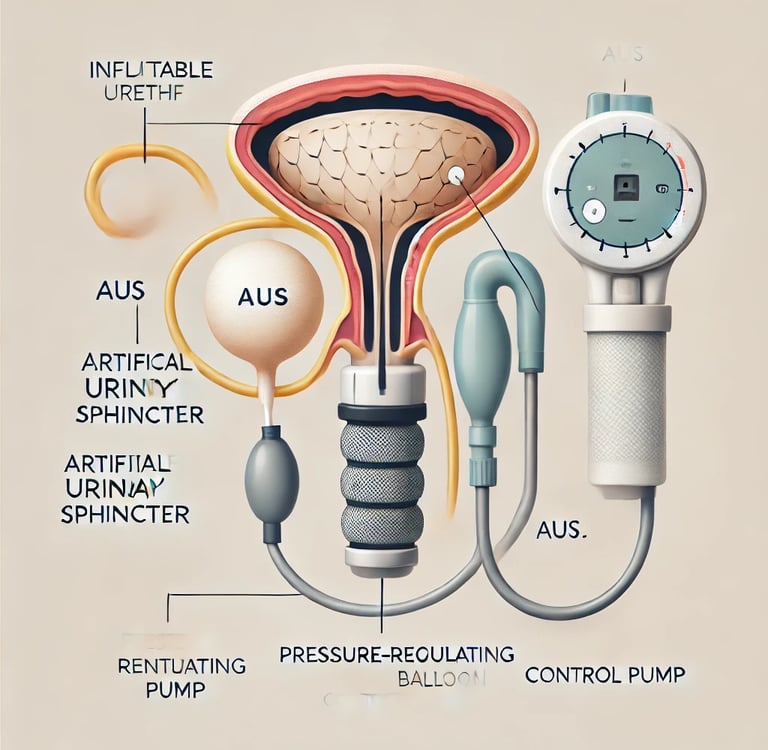
The mechanism of artificial urinary sphincters relies on a fluid-filled cuff, which is typically placed around the urethra. This cuff can be inflated or deflated using a pump located in the scrotum or labia, allowing the patient to control their urination. When the cuff is inflated, it compresses the urethra, preventing the flow of urine. Conversely, deflating the cuff permits urination. The design aims to mimic the natural functionality of human urinary control, providing patients with autonomy over their bladder function.
Medical conditions that commonly justify the use of an artificial urinary sphincter include postoperative complications from prostatectomies, congenital anatomical abnormalities, and neurological disorders, such as multiple sclerosis or spinal cord injuries. These conditions can lead to significant discomfort, embarrassment, and lifestyle limitations, making the surgical intervention offered by an AUS a vital aspect of patient care.
As illustrated below, proper placement and functioning of the artificial urinary sphincter are crucial to its effectiveness. Understanding this device's anatomy not only highlights its significance in urological care but also aids in patient education regarding the procedure and expected outcomes. The integration of artificial urinary sphincters into treatment regimens signifies a commitment to enhancing patient quality of life while addressing the complexities inherent to urinary incontinence management.
Available Brands and Manufacturers
When it comes to artificial urinary sphincters (AUS), several well-known brands and manufacturers dominate the market, each offering distinct features. One of the most recognized brands is the AMS 800 by Boston Scientific. This device is designed to control urinary incontinence through a three-component system: a pressure-regulating balloon, a cuff, and a pump. The AMS 800 is known for its reliability and ease of use, although some patients may experience issues with the device's bulkiness or the need for surgical adjustments.
Another prominent manufacturer is Coloplast, which produces the Atos Device. The Atos Device stands out due to its lightweight construction and flexible design, which may provide enhanced comfort for users. However, it can be slightly less durable in certain conditions compared to competitors. Coloplast also emphasizes patient education and support, providing resources to ensure optimal function of their devices.
Innovative Medical Devices is a newer but notable entrant in the market with their product known as the Urethral Sphincter. This device aims to offer a more customizable solution for patients, allowing for adjustments that cater to individual needs. While the variability in the product could be advantageous, there may be limited long-term data on its effectiveness, which can be a point of concern for potential users.
Accessibility of these devices fluctuates by region, with manufacturers often having different distribution channels. In North America, AMS 800 is widely available across hospitals and specialized clinics, while Coloplast products may have wider access in Europe. Patients should consult their healthcare providers for specific availability and whether their insurance covers these devices, ensuring they make informed choices regarding their treatment options.
Alternative Interventions and Options
Urinary incontinence can significantly impact an individual’s quality of life, leading many to seek effective treatments beyond artificial urinary sphincters. A variety of alternative interventions are available, catering to different causes and severities of incontinence. Understanding these options is crucial for those who may not have access to surgical solutions such as artificial urinary sphincters.
One of the primary alternatives includes the use of medications. Certain pharmacological treatments aim to improve bladder control by adjusting the levels of neurotransmitters responsible for bladder function. Anticholinergic medications and beta-3 agonists are among the options that may help minimize incontinence episodes by reducing involuntary bladder contractions or increasing bladder capacity. However, medications may carry side effects and may not be suitable for everyone, making a thorough consultation with a healthcare provider essential.
Another effective intervention involves pelvic floor exercises, commonly known as Kegel exercises. These exercises focus on strengthening the pelvic floor muscles, which can support the bladder and enhance control over urination. Regular practice of pelvic floor exercises has been shown to improve symptoms of stress and urge incontinence over time. This non-invasive method is especially advantageous for those looking to avoid surgical procedures.
Surgical interventions, aside from artificial urinary sphincters, offer additional options for managing urinary incontinence. Procedures such as mid-urethral sling surgery or bladder neck suspension manipulate the anatomical structures supporting the bladder, providing increased stability and control. Each surgical option has varying levels of invasiveness and recovery time, and they generally come with associated risks that should be discussed with a healthcare professional.
In summary, while artificial urinary sphincters are a specific intervention, various other treatment modalities exist for managing urinary incontinence. Medications, pelvic floor exercises, and surgical interventions can provide effective solutions tailored to individual needs, potentially improving the overall management of urinary symptoms.
Cost and Accessibility Overview
The cost of artificial urinary sphincters can vary significantly based on factors such as the brand, the geographic location of the purchase, and any associated medical procedures. Generally, the price tag for these devices ranges from $4,000 to $10,000. This variability stems from differences in device complexity, the technology utilized, and the specific features offered by manufacturers. Leading brands, such as the AMS 800 and the Mentor Alpha I, may command higher prices due to their established reputation and proven efficacy.
In addition to the device costs, patients should also consider the potential expenses related to the surgical implantation of the sphincter. Surgical fees, anesthesia, hospital stay, and post-operative care can accumulate, increasing the total financial burden. Costs associated with follow-up care and maintenance of the device should also be factored in, as ongoing monitoring and potential adjustments could be necessary over the lifespan of the sphincter.
Geographic location plays a significant role in determining accessibility as well. Costs can vary based on the region, with urban centers often reflecting higher pricing due to increased healthcare operational costs. Moreover, healthcare policies, insurance coverage, and reimbursement procedures significantly influence how individuals access these devices. Some insurance policies might cover a portion of the costs, while others may classify artificial urinary sphincters as experimental, leaving patients with substantial out-of-pocket expenses.
The economic aspect of artificial urinary sphincters can present challenges for patients needing these devices. Therefore, fostering conversations about personal experiences and obstacles related to financing or obtaining these medical aids can be beneficial. Sharing insights within a community not only raises awareness but might also provide solutions for navigating cost and accessibility issues in the realm of artificial urinary sphincters.
