Anesthetic Delivery Devices for Regional Blocks: Innovations and Applications
4/6/20254 min read

Understanding Regional Anesthesia
Regional anesthesia plays a vital role in contemporary medical practices, offering effective pain relief during and after surgical procedures. This approach involves the administration of anesthetic agents to specific blocks of nerves, thereby providing targeted analgesia while minimizing systemic effects associated with general anesthesia. By focusing on specific regions of the body, regional blocks allow patients to experience reduced pain and quicker recovery times, making them an appealing choice for many surgical interventions.
Commonly employed types of regional blocks include brachial plexus blocks for upper limb surgeries, femoral nerve blocks for knee surgeries, and sciatic nerve blocks for ankle and foot procedures. Each regional block caters to different anatomical areas, providing significant benefits. For instance, these blocks can enhance postoperative pain management, facilitate patient mobility, and decrease the need for complementary opioid analgesics, leading to a lower risk of side effects.
Understanding the anatomy relevant to regional anesthesia is crucial for practitioners aiming to achieve optimal outcomes. Insight into the anatomical landmarks ensures the precise delivery of anesthetics to the targeted nerves, thereby enhancing the efficacy of the block. Familiarity with nerve pathways and adjacent structures not only improves the success rate of the procedure but also minimizes potential complications. Additionally, advancements in imaging technologies such as ultrasound guidance have revolutionized the administration of regional anesthesia, allowing for improved visualization of nerves and decreasing the likelihood of unsuccessful blocks.
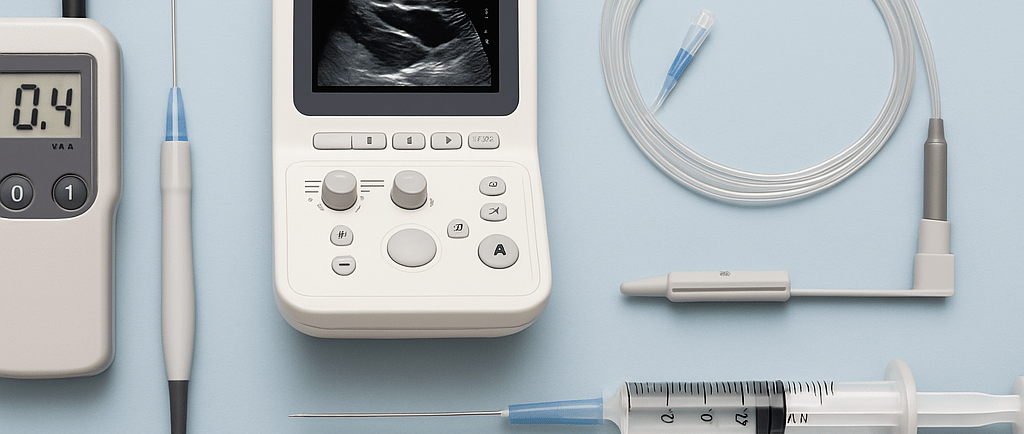
The evolution of anesthetic delivery devices has further contributed to the enhanced safety and efficacy of regional anesthesia. These innovations promote better drug dispersion and facilitate accurate dosing, ultimately leading to improved patient outcomes. In a medical landscape that increasingly favors minimally invasive techniques and personalized approaches to care, regional anesthesia continues to assert its significance, underscoring the importance of targeted pain management strategies in modern surgical practices.
Innovations in Nerve Stimulators
Nerve stimulators have undergone significant evolution over the years, enhancing the process of regional anesthesia through precise targeting of nerve pathways. These devices utilize electrical impulses to locate and stimulate specific nerves, enabling practitioners to ascertain the most accurate injection sites for local anesthetics. This precision not only increases the effectiveness of nerve blocks but also contributes to a reduction in the risk of complications associated with regional anesthesia.
The working mechanism of nerve stimulators is based on the depolarization of nerve fibers, which results in muscle contractions or twitching that indicate proximity to the targeted nerve. Traditional models of nerve stimulators provided basic functionality; however, advancements have led to the development of programmable nerve stimulators. These modern devices feature adjustable parameters, allowing clinicians to customize stimulation intensity and frequency according to individual patient needs, further enhancing accuracy during procedures.
One of the primary benefits of these advancements is the significant reduction in patient discomfort. By accurately identifying nerve locations, healthcare providers can minimize unnecessary needle insertions and ensure that anesthetic administration is as comfortable as possible. Additionally, improved accuracy facilitates better outcomes in surgical settings, contributing to enhanced patient safety and satisfaction. Recent innovations have also seen the integration of ultrasound technologies with nerve stimulators, offering real-time visualization that augments the precision of nerve localization.
The clinical implications of these advancements in nerve stimulators are vast. In orthopedic, obstetric, and various other surgical procedures, enhanced accuracy and safety translate into more effective pain management strategies. As the field of anesthesiology continues to evolve, the integration of innovative nerve stimulators represents a significant leap forward in the practice of regional anesthesia.
Ultrasound-Guided Anesthetic Delivery Devices
The integration of ultrasound technology into regional anesthesia represents a significant advancement in anesthetic delivery devices, facilitating improved precision in block placement. This innovative approach utilizes real-time imaging to enhance the visualization of nerves and surrounding anatomical structures, thereby allowing practitioners to navigate complex anatomical landscapes with greater accuracy. The adoption of ultrasound guidance in regional blocks has led to marked improvements in success rates, with studies indicating a substantial reduction in complications associated with traditional blind techniques.
Traditional methods of regional anesthesia often rely on anatomical landmarks, which can be subjective and lead to variability in successful outcomes. In contrast, ultrasound guidance provides a dynamic and reliable method of identifying target nerves and adjacent tissues, minimizing the risk of intravascular injection or inadvertent damage to surrounding structures. This precision is particularly advantageous in procedures such as brachial plexus blocks, femoral nerve blocks, and sciatic nerve blocks, where anatomical variations can complicate the anesthetic delivery process.
Numerous case studies illustrate the practical benefits of ultrasound-guided techniques. For example, a multicenter analysis revealed that patients receiving ultrasound-guided blocks experienced lower rates of block failure and fewer adverse events compared to those undergoing landmark-guided procedures. Moreover, the ability to visualize the spread of local anesthetic in real time allows clinicians to adjust their technique on-the-spot, ensuring optimal delivery of anesthetic agents. The use of ultrasound not only enhances the efficacy of regional anesthesia but also contributes to improved patient satisfaction due to reduced pain and increased safety during surgical interventions.
As the field continues to evolve, the advancements in ultrasound-guided anesthetic delivery devices will likely lead to further improvements in the quality of care and outcomes for patients undergoing procedures requiring regional anesthesia.
Advancements in Drug Delivery Innovations
Recent advancements in drug delivery systems have significantly transformed the landscape of regional anesthesia, enhancing patient outcomes through improved analgesic efficacy and duration. One notable innovation is the use of liposomal bupivacaine, a formulation designed to provide prolonged pain relief compared to traditional bupivacaine. This liposomal encapsulation facilitates a controlled release of the analgesic around the nerve, thus extending the duration of action and reducing the need for supplemental analgesics. Such innovations enable a more focused approach to pain management and have the potential to enhance postoperative recovery.
Another promising avenue in drug delivery involves microparticle-based systems that encapsulate anesthetic agents. These systems not only prolong the release of analgesics but also allow for targeted action at specific sites. Such targeted delivery mechanisms can minimize systemic exposure, thereby reducing the potential for side effects and improving the safety profile of anesthetics. By utilizing these advanced technologies, practitioners are better equipped to offer tailored pain management solutions that align with individual patient needs.
Controlled release technologies are gaining traction as they offer the ability to maintain therapeutic drug levels over extended periods. This can be particularly beneficial in the context of regional blocks, where consistent analgesia is paramount for patient comfort and recovery. Furthermore, the incorporation of patient-controlled analgesia systems into regional anesthesia protocols empowers patients, allowing them to manage their pain more effectively and respond to their unique pain thresholds.
As we look to the future, the integration of these cutting-edge drug delivery innovations into clinical practice presents exciting possibilities. The continuous evolution of anesthetic formulations and delivery systems promises to redefine pain management strategies, ultimately leading to safer and more effective patient-centered care. These advancements not only enhance the quality of postoperative recovery but also have the potential to reshape the standard practices in regional anesthesia, ensuring better outcomes for patients undergoing various surgical procedures.
